Hello and welcome to ProbioticAdvisor.com!
ProbioticAdvisor.com provides independent, unbiased, evidence-based information on probiotics, their potential risks, and documented benefits.
The recent explosion of research on probiotics, combined with the sheer multitude of probiotic products in the marketplace, has made it challenging to navigate through competing product’s claims of superiority.
Hence, there is a great need for industry-independent, evidence-based resources on probiotics to help guide clinical practice.
To meet this need, Dr Jason Hawrelak – probiotic researcher, educator, and clinician – created ProbioticAdvisor.com and more specifically, the Probiotic Advisor.
ProbioticAdvisor.com has been designed with a number of aims in mind:
Firstly, to provide health professionals and consumers with the background knowledge needed to become more critical consumers of probiotic products. Both practitioners and consumers need the right background knowledge to enable them to ask the right questions so they can successfully navigate through the probiotic information minefield – an area where many sources of information are biased or prepared by individuals without specialized knowledge of probiotics.
The second aim is to help clinicians prescribe probiotics in a more evidence-based manner. The utilization of probiotics as therapeutic agents is a relatively 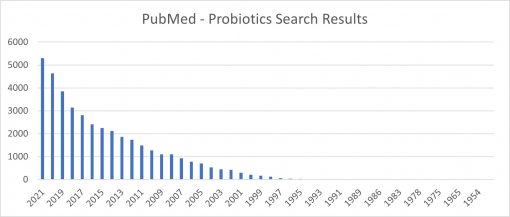 new and quickly-evolving field. Consequently, it can be hard for clinicians to keep up with the pace of the research (see graph to the right). When I first started researching probiotics as part of my Honours degree in 2000, it was possible to read all of the research that was published in the probiotic field in that year (with just over 200 papers published). But in 2021, there were nearly 5,000 papers published – a challenging amount to read and digest for fulltime researchers, let alone busy clinicians!
new and quickly-evolving field. Consequently, it can be hard for clinicians to keep up with the pace of the research (see graph to the right). When I first started researching probiotics as part of my Honours degree in 2000, it was possible to read all of the research that was published in the probiotic field in that year (with just over 200 papers published). But in 2021, there were nearly 5,000 papers published – a challenging amount to read and digest for fulltime researchers, let alone busy clinicians!
The growth in probiotic research has been paralleled by an increase in the number of probiotic preparations available commercially. There is now a substantial number of probiotic preparations in the marketplace – all claiming superiority.
What makes a good probiotic supplement?
How do you differentiate the superior from the inferior?
How can you determine the best choice of probiotic supplement for a patient? Or the brand most likely to be effective for a specific health condition?
At ProbioticAdvisor.com, we’ll provide you with the background knowledge needed to make the right choices and provide the best advice to your clients.
We’ll also introduce you to the Probiotic Advisor – a powerful tool that will revolutionize your use of probiotics.
With this tool you can quickly critique probiotic preparations, look to see if, and in which product, a well-researched probiotic strain can be found, and locate the strain(s) with the best evidence to treat the condition at hand. So far we’ve included probiotic preparations available in Australia, Canada, and the US.
You’ll soon wonder how you ever practiced without it!
There is a lot of information on probiotics available online. Much of it, however, is of questionable accuracy, comes from biased sources, or is written by individuals without specialized knowledge on probiotics.
ProbioticAdvisor.com is different – the information is independent, unbiased, evidence-based, and written by individuals that have extensive and specialist knowledge on probiotics.
Our hope is that you’ll find the information on ProbioticAdvisor.com practice-changing!
Best regards,
Dr Jason Hawrelak
On Behalf of the Probiotic Advisor Team
